Three years ago, everything changed. That’s when COVID-19 began a deadly rampage that has left millions around the world dead and many more lives irreparably changed.
The healthcare industry, as the front line of defense against the deadly virus, bore the brunt of the attack, and it has been obvious that with respect to security — of people, buildings, equipment — things were going to change and change dramatically.
The pandemic continues to rage, although at lower levels and away from the spotlight of 2020 or 2021, but enough distance has come between the start of COVID and now that it’s possible to assess how COVID has affected healthcare security and what’s to come.
Locksmith Ledger recently discussed the issues of postpandemic healthcare security with several industry experts. The participants include Tom Morgan, director of business development-healthcare at ASSA ABLOY Opening Solutions; Justin Lockhart, assistant vice president of sales, central region for dormakaba Americas; Bryan Warren, president of WarSec Security; Michael Dunning, principal consultant, The Healthcare Security Consulting Group; and Robert Massard and David Boilore, president and general manager, respectively, of Redford Lock Security Solutions in Novi, Michigan.
Q: How has COVID affected security at healthcare facilities?
Tom Morgan: With the flu season underway, RSV at new levels and lingering pandemic infections, healthcare workers are again stretched thin. The extra workload, hours and stress have led to burnout for many as well as staffing shortages. Further straining the system are alarming cybersecurity issues and the disturbing side effect of healthcare workplace threats from upset or agitated patients, family members and criminals.
Justin Lockhart: Three areas were affected. First and foremost was people management, which involved managing the physical security and hygiene safety of the patients themselves, so they could be treated while limiting exposure. The next effect was on maintenance for increased security systems and protocols without compromising ease of access for visitors and healthcare workers. Finally, compliance required the constant evaluation of any access solutions, security changes and system integrations to assure code compliance for ingress and egress.
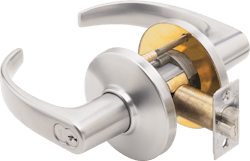
From a product standpoint, the use of touchless access solutions increased significantly to reduce the spread of contagions. In addition, we saw an increased use of other electrified solutions that tie into the property-management system, such as electrified locksets, panic devices that have motorized latch retraction, electrified mechanical hardware and the use of credentialed door hardware, among others. We also saw an increased interest in using antimicrobial mechanical door hardware when possible to help to limit the spread of germs.
Bryan Warren:The pandemic has had significant effects upon the healthcare industry, as one can imagine. Day-to-day challenges with securing a healthcare environment were enhanced because of the restrictions that COVID placed upon the operations of these hospitals and patient-care areas. In addition, stress levels increased not only in patients but also in caregivers because of staffing shortages and the overall concern for their own well-being. This has resulted in an increase in incivility and acts of workplace violence. There also has been an issue with many facilities restricting visitation, which further complicates an already emotionally charged environment.
Michael Dunning: COVID can be felt on a few different levels and, in some respects, has had a domino effect.
First, there has been a decrease in the number of people going to healthcare facilities. Although this is starting to return to pre-COVID numbers, the number of people visiting doctors for routine checks, elective surgeries and other procedures has declined. This decline has had a significant effect on the financial well-being of healthcare facilities.
Second, the overall effect of increased anxiety and fear among the general population, paired with increased restrictions on visitation and requirements for entering healthcare facilities, has led to decreased tolerance levels and patience and increased levels of violence in healthcare facilities.
The increase in violent behavior added to the overall increases in anxiety, and fear has led to fewer people wanting to work in healthcare facilities. This includes clinical and support positions, which lowers the capability of healthcare facilities to provide services, increases the demands and stress levels of staff and increases the financial pressure on facilities to meet the increased demands of higher pay rates.
To put it simply, it has become more difficult to hire and retain security officers in healthcare facilities.
Robert Massard: Early on, everyone was concerned about “antimicrobial,” and there was a lot of buzz about it, but no one really did anything. The most I saw anyone do was mount hardware at the bottom of the door to open your door with a foot. It was a fad, and everyone was trying to throw bandages at everything.
I can’t say anyone is doing anything differently. They’re still doing their fire-door inspections. They’re still doing their repairs, but that started before the pandemic, and that’s still more of a hot button to [hospitals].
Q: With respect to physical security, what changed, what will change and what should be changed?
Morgan: A healthy, secure and safe environment is more important than ever in helping to promote healing and yielding better outcomes for patients. The better the safety and security measures, the more doctors and nurses can stay focused on giving patients the best care possible, and the better the chances are for retaining and recruiting staff.
Coinciding with the increased demands and stressors on the healthcare workforce is the rise in hospital and clinic construction. Notably, behavioral-health and psychiatric facilities continue to make up the highest percentage of expansions underway or being planned over the next few years. Many include dedicated treatment centers within hospitals, as well as behavioral-health emergency intake or triage areas separate from main emergency departments. These discrete facilities provide an extra level of privacy, safety and healing efficacy for the patient as well as further protection for healthcare staff.
Lockhart: Since COVID, there has been a growing convergence of electronic access solutions and mechanical hardware. As we move forward, security consultants and architectural hardware consultants will collaborate earlier and more often. This alignment is critical for a facility to achieve its security goals. When the two parties are aligned, they can address security and convenience requirements efficiently and thoughtfully. The end result is that end users now have a total-openings solution that meets healthcare security requirements as well as life safety, ADA and other code compliances in the best ways possible.
Warren: As mentioned, visitation and entry dramatically changed because of COVID and the necessity of screening protocols for everyone who enters a healthcare facility, including staff. This resulted in previous ingress points being closed and people being rerouted to “funnel” them through screening checkpoints.
At first, this was quite chaotic, particularly for facilities that didn’t restrict access or visitation in some form. Over time, hospitals became more adept in effective and efficient screening procedures, and many implemented visitor badges and other temporary forms of ID to demonstrate a person had been screened and what their purpose was for being inside the facility.
This process, which was born out of necessity, will become more commonplace. This will improve overall security for many facilities, because those who might visit a hospital for criminal purposes now will have to go through some form of identification process, and anonymity won’t be as easy for them as before. Healthcare administrators have to be educated regarding how much of an effect physical-security investments can have in providing a quality patient-care outcome while protecting caregivers.
Dunning: The way we look at physical security is starting to change. In the past, the mindset for security programs was reactive. As we move forward, a more proactive approach to preventing incidents from occurring by earlier detection of escalating behaviors and employing deterrence tools will be necessary.
Proactive, layered access control is key in early detection by managing who accesses the facility and controlling that access.
Training staff for situational awareness and de-escalation will be necessary, along with identifying thresholds and communication protocols to summon assistance when escalating behavior is detected. This alters the response from a physical “bully” tactic to a more patient-centric targeted response.
Using cameras and other detection systems that have artificial intelligence will help to identify behaviors and weapons upon entry, which provides early detection and quicker response.
David Boilore: Procedural security changed temporarily, and that was in regard to everyone having to enter the facility though one particular access point to be screened, which since has been dropped by many facilities.
I have no guess as to what will change. However, hospitals being 24-hour facilities creates a unique challenge to security. I would recommend continuing to funnel most visitors and vendors through one access point to ensure they’re on-site for healthcare purposes or support and not freely roaming the hospital with bad intent.
Q: As a result, what products or systems will play a major role in this market?
Morgan: Many, covering several categories.
Door Solutions. Digital access solutions, or electronic access control (EAC), continue to provide some of the most effective ways to keep healthcare facilities safer, preventing unauthorized entry into sensitive departments, care units and supply rooms. Controlled-egress doors prevent escape from treatment areas where the clinical requirements of patients require their containment, such as behavioral-health or memory-care units, or an infant patient-care wing, where the release of a child must be monitored and managed carefully.
Digital access solutions also are being integrated more into nondoor applications, such as locks for pharmaceutical storage, server rack doors and patient file cabinets. Along with tightening authorized access and security to these vital assets, EAC provides audit trail data for more accountability wherever the technology is used.
Many facilities are updating door security by rekeying openings and using patented or electronic keyways and e-cylinders.
For behavioral-health applications, solutions also include specialized patient-room access doors, double-swing hinges that have emergency release stops and ligature-resistant door hardware.
Touchless Solutions. Preventing the spread of germs always has been critical in healthcare safety. Hands-free door solutions play a key role in that prevention. Although many facilities had been installing these solutions prior to the pandemic, the demand for wave-to-open and other automatic door solutions has shot up since, even though COVID and flu viruses are spread primarily through the air. Low-touch hardware, such as arm paddles and foot pulls and antimicrobial or antiviral surface treatments for levers and pulls have become ubiquitous as well.
Along with promoting health and safety, these hands-free products provide extra convenience by allowing staff and the public to pass more freely through openings. This is particularly helpful for those who have mobility issues and other disabilities as well as healthcare workers who move patients, equipment and armfuls of supplies.
Cybersecurity. Threats also extend to cyberattacks, which have increased significantly worldwide since COVID entered our lives.
Originally, cybersecurity was about safeguarding computers and servers. Today, the focus is on the cybersecurity of networks and the increasing number of interconnected IoT devices, including those that provide physical security, such as digital access solutions for door openings in healthcare facilities.
We get questions and surveys from security pros and end users all the time inquiring about how robust our products are in standing up to cybercriminals. We’re vigilant about leveling up to the evolving cyberthreat landscape.
Lockhart: Among the most important products and systems will be EAC systems that manage credentialed ingress and egress with no performance-limiting or system-expansion governors. These products provide robust system-integration capabilities that respond to immediate access demands and set the stage for future scalability.
The use of antimicrobial mechanical locks will continue to be important to help to reduce the spread of contagions. Mechanical locks aren’t likely to go away, and they remain a low-cost security option in some specific use-case scenarios. Using a mechanical lock that has an antimicrobial finish expands the lock’s capability by adding an element of hygiene safety.
Electrified hardware for touchless commercial openings will continue to be popular options for buildings where managers want to reduce the spread of germs in high-traffic areas. Touch-free is here to stay, and many employees and guests expect such options to be present in our new era of heightened hygiene sensitivity.
In addition to door hardware, entrance systems will be key contributors to a healthcare facility’s security and wellness plan and increase in relevance. A smooth entrance system manages traffic flow, preserves indoor climate and maintains security and access into a building.
Warren: Access controls that can be integrated easily into existing systems will be significant, as well as enhancements to screening at entry points — for example, taking existing COVID screening processes and adapting them to include metal detection or weapons screening. Visitor-management process, systems and related products also will continue to see growth as facilities adapt to this shift in expectations. Items that once were considered uncommon, such as video analytics directly tied into access controls, portable duress alarms for clinical staff and body-worn cameras for security personnel, are becoming more common as the technology and cost of implementation decrease. Healthcare leaders are starting to better understand that security measures are an investment and not just a cost.
Dunning: Early detection systems, such as more-advanced weapons detection and camera systems that can detect escalating behaviors, will be necessary at entrances, areas of high traffic and areas of increased concern, such as behavioral-health and emergency departments.
The ability to coordinate and integrate security systems will be necessary. The ability to secure areas on demand is necessary to protect staff during incidents of violence, particularly during an active-shooter event. But these mechanisms also will have to accommodate people who want quick entry into areas.
Massard: Hands-free. Hands-free wall switches for operators. More card access. Antimicrobial specifications for door hardware. That’s not something you can do readily, because nobody really stocks antimicrobial product. The manufacturers can make it, and they do market it, but it takes quite a while to implement it — and it’s a little bit pricey, but you definitely will see more of that. I don’t want to say we’re becoming germaphobes; we’re trying to be prepared.
Q: What should locksmiths know about this new environment, and how should they best prepare themselves to participate?
Morgan: Healthcare facilities are counting on your ability to deliver the highest quality workmanship to help to ensure their occupants’ security and safety.
Although there are an increasing number of facility expansions that include digital access solutions, healthcare budgets might tighten in the coming year considering the potential of a recession that still exists. That could lead to more emphasis on cost-effective options, such as lock retrofits for existing facilities. In either case, the healthcare industry has to maximize its investment, which includes procuring the best in product functionality and reliability, solutions knowledge and quality installation.
Security and facility managers, architects and end users look for a high level of comprehensive expertise among security pros. So, it’s essential to keep up with the latest door hardware and digital access options. It’s also important to pay close attention to the decorative and ergonomic advancements that have become important in improving the healing environment and accessibility.
Lockhart: Access control solutions and integrations are increasingly common pieces in the overall security and safety puzzle for any healthcare building. Although it’s important to maintain critical knowledge of mechanical locks and keys, today’s locksmiths must become well-versed in total opening solutions to best serve their customers.
The best way to do that is to invest in training to stay up to date on the latest advances in healthcare security. Manufacturers provide a variety of in-person and digital training programs. In addition, tech updates from manufacturers, trade media, trade events and trade memberships can help locksmiths to become the best people to service healthcare customers today and tomorrow.
Dunning: The healthcare environment is filled with regulatory requirements, from fire codes to space identification, that create additional layers to navigate when developing security programs and access control. Those requirements can change from a federal and state level. and from facility to facility, based on which accreditation agency is used. Knowledge of those requirements and the ability to stay current will be key in providing the tools healthcare facilities will want.
Boilore: I would recommend keeping apprised of new products that provide a more hands-free solution for door hardware. Also, typically, small facilities have nonrestricted or nonpatented master-key systems. A proper key system is always a sound investment for any site to protect against the unauthorized duplication of keys. This also reduces the sharing of keys with others who shouldn’t be entering restricted areas and creates accountability, because good record-keeping will show who had access to an area where damage or theft has occurred.
Massard: Knowledge. Knowledge is still the key. A lot of locksmiths don’t call on these facilities. If you don’t, you should go out and educate yourself — just visit some of these sites, grab a seat in the lobby and watch what’s going on. Do some studying on codes — specifically, life safety and security.
And what’s good for hospital system ABC might not be good for the one down the street, because they have different policies and procedures. Know your customer. I guess that’s kind of an old, golden rule, but it still applies.
Will Christensen | Senior Editor
Will Christensen is senior editor at Locksmith Ledger International. He has been an editor and reporter at magazines and newspapers for more than 30 years.